Few predictive factors for symptomatic progression of gallstone disease:
- Bariatric surgery - 30% develop gallstones
- post-colectomy - 20% will develop symptoms within 5 years
- prolonged TPN use
Despite these risk factors, there are few indications for prophylactic cholecystectomy:
- Expectant Management of Cholelithiasis is the accepted treatment despite low morbidity of lap chole
- Diabetes is not an indication for prophylactic chole. Diabetics do not have any significant difference in prevalence, presentation or complications compared to nondiabetics
Post-Transplantation:
- Cyclosporine leads to gallstone formation.
- Need for prophylactic chole has been shown to be of benefit in cardiac transplant patients if screening u/s shows stones (Milas et al, Mayo clinic)
- in renal transplant patients, majority (~90%) remain asymptomatic
Hemoglobinopathies:
- at risk of developing pigmented stones.
- sickle cell: 70% of pts
- hereditary spherocytosis: 85%
- thalassemia: 24%
- Gallstones in sickle cell patients can pose a problem. ~50% will become symptomatic within 3-5 years. Presence of gallstones can be diagnostically challenging due to possibility of abdominal sickling crisis.
- Hemoglobinopathies are an indication to perform prophylactic lap chole, lap chole should also be performed if doing a lap splenectomy
Bariatric Surgery:
- incidence of gallstone formation after rapid weight loss:
- general population: 10-20%
- bariatric surgery population: 30-40%
- if gallstones documented at time of bariatric surgery - lap chole recommended
- Ursodiol - can decrease incidence if patient compliant (prevents cholesterol absorption, expensive (~$1.50/d), BID). Suggested for patients undergoing bariatric surgery without prior evidence of stones.
Incidental Cholecystectomy - Controversial:
- During AAA: controversial due to the presence of graft material. Review of incidental chole - shown to be safe as long as performed after retroperitoneum is closed
- Other abdominal surgeries: One study (Watemberg et al) showed that in pts >70 yo with cholelithiasis, M&M was higher if you DO NOT do incidental chole during laparotomy for other reasons.... yet we do not routinely do this in practice - why?
- most were small studies - only Watemberg was larger study
Thursday, January 21, 2010
Wednesday, January 20, 2010
CBD injuries
Strasberg classification CBD injuries
Sent from iPhone
Sent from iPhone
Tuesday, January 19, 2010
Gallbladder Polyps
Prevalence GB Polyps: 3-10%
Differential:
- Cholesterol polyps (50-70%)
- inflammatory
- hyperplastic
- adenoma
- malignant (8%)
Predictive factors for malignancy:
- size >1cm
- broad based sessile polyps
- age >50
Treatment:
- suspicion for GB cancer low: lap chole
- suspicious for GB cancer: open chole with intraop frozen section
- small polypoid lesion: U/S q6 mo for 2 yrs to ensure stable lesion
Differential:
- Cholesterol polyps (50-70%)
- inflammatory
- hyperplastic
- adenoma
- malignant (8%)
Predictive factors for malignancy:
- size >1cm
- broad based sessile polyps
- age >50
Treatment:
- suspicion for GB cancer low: lap chole
- suspicious for GB cancer: open chole with intraop frozen section
- small polypoid lesion: U/S q6 mo for 2 yrs to ensure stable lesion
Gallbladder Cancer
T1a GB Ca: usually early stage
- usually found incidentally after routine lap chole
- incidence after routine lap chole for cholelithiasis - 1-2%
- 5 year survival for T1a GB ca confined to the mucosa - 85-100%Symptomatic patients: usually advanced stage
- U/S only 50% sensitive for GB ca
- if suspicion of GB cancer pt should have a CT scan or MRI to look for invasion into adjacent structures, LN or encasement of portal vein or hepatic artery.
- Other investigations to consider: PET, MRCP, ERCP
Treatment is based T-stage of the tumor
- contraindications to surgical resection: liver mets, malignant ascites, peritoneal mets, distant disease, extensive involvement of hepatoduodenal ligament, encasement or occlusion of major vessels, poor performance status.
Lap Chole:
Tis or T1a
Radical Cholecystectomy:
-T1b (15% subserosal LN involvement) or T2 (40-80% subserosal LN involvement)
- radical cholecystectomy involves resection of GB with a 2cm hepatic parenchymal margin and LN dissection within the porta hepatis, gastroduodenal ligament, gastrohepatic ligament and Kocher for LN dissection behind duodenum
- can be done at time of initial lap chole or can be delayed - survival the same
- can be done at time of initial lap chole or can be delayed - survival the same
Radical Cholecystectomy +/- en bloc resection of locally invaded organs:
- advised for T3/T4 tumors only if there is no evidence of metastatic spread
- 25-44% 5 year survival rate
Palliation:
- survival in locally unresectable or metastative disease often <1 yr
- no effective adjuvant treatment - all part of clinical trials
Palliation:
- survival in locally unresectable or metastative disease often <1 yr
- no effective adjuvant treatment - all part of clinical trials
Friday, January 15, 2010
Hepatocellular Carcinoma
Hep C is highest risk factor worldwide of HCC (>50% in NA)
- any type of cirrhosis carries risk of HCC
- what about Hep A (or is it only chronic Hepatides)
Screening in cirrhotic pts important:
- clinical presentation will be late in disease process
- AFP, U/S q6 months
- any solid liver nodule not clearly a hemangioma should be considered an HCC in a cirrhotic pt until proven otherwise
REsection
Child PUgh A - normal bili, INR, albumin, no encephalopathy, no ascites
unilobar
no major co-morbidites
Malignant liver tumors
American Associatiion of Liver Disease HCC diagnostic criteria
- ?
- main point is that FNA not necessarily required for diagnosis and may track tumor in needle site converting treatable lesion to untreatable
Treatments for HCC
Curative:
- TRansplant
- resection
- Radiofrequency ablation
Palliative
- TASTE (embolization)
- chemotherapy
Best treatment modality HCC:
- Transplant (treats both tumor underlying liver dysfunction)
- resection has 50% 5 year survival (largely from liver disease and risk of 2nd primary)
Factors for HCC resection
- liver function
- tumor characteristics (number, size, multifocality)
Primary liver tumors:
HCC
cholangiocarcinoma
malignant vascular tumors (epitheliod hemangioendothelioma, angiosarcoma)
sarcomas (embryonal sarcoma, ...)
Most common sources of liver mets (hypoattenuating):
Colorectal, Breast, Lung
Hyperattenuating:
- melanoma, renal cell
Treatment goals:
- R0 resection
- preserve ~25% hepatic parenchyma
- adjuvant or neoadjuvant chemoRT to reduce risk recurrence
Benign liver lesions - AHD
3 most common benign liver lesions:
1) Adenoma
2) FNH
3) hemangioma
Factors for resection:
- symptoms (chronic, aching pain under the right costal margin, constant)
- type (adenomas carry malignancy risk, FNH do not)
- location (peripheral hemangioma at risk of rupture)
- growth (compression of biliary/vascular strucutres)
Pancreatic cancer
Indications preop stents.
Acute cholanfitis
Intense puritis
Neoadjuvant chemotherapy
- short length self expanding stent
Management of nonresectable cancers
- ercp and stent
- PTC mettalic stent if no ercp access
- Eus or us guided fna biopsy possible celiac plexus block
- if associated gastric outlet obstruction then double bypass or
duodenal stent
Operative management
- Any metastatic disease in pancreatic cancer - the patient is
unresectable
- staging laparoscopyuswd in some institutions but low yield
If non-resectable
- Trans duodenal trucut pancreatic biopsy
- palliative
Sent from iPhone
Acute cholanfitis
Intense puritis
Neoadjuvant chemotherapy
- short length self expanding stent
Management of nonresectable cancers
- ercp and stent
- PTC mettalic stent if no ercp access
- Eus or us guided fna biopsy possible celiac plexus block
- if associated gastric outlet obstruction then double bypass or
duodenal stent
Operative management
- Any metastatic disease in pancreatic cancer - the patient is
unresectable
- staging laparoscopyuswd in some institutions but low yield
If non-resectable
- Trans duodenal trucut pancreatic biopsy
- palliative
Sent from iPhone
Monday, January 11, 2010
Calcium replacement post-op hypocalcemia
Elemental calcium 2-4g per day +\- rocalcitrol 0.25 ug qd
Calcium carbonate: (1g CaCarbonate has 400mg elemental calcium)
If symptomatic 1 amp calcium gluconate in 50ml d5w over 20 min
Replace magnesium
Calcium carbonate: (1g CaCarbonate has 400mg elemental calcium)
If symptomatic 1 amp calcium gluconate in 50ml d5w over 20 min
Replace magnesium
Tuesday, January 5, 2010
Exposure Abdominal Aortic Aneurysm
1) Draping: shave abdo and groins, knees to nipple prep, groin drape and square offs, ioban over abdomen
2) Midline incision from xiphi to pubis
3) Check placement of NG
4) Find and divide LT and mobilize 4th part of duodenum by dividing filmy attachment between duodenum and inferior mesenteric vein
5) Place bookwalter or omni with right sided bias as most contents will be retracted that way
6) Retract tranverse colon by placing splancnic retractors to also retract duodenum and IMV
7) Place large maleable retractor at base of small bowel mesentery and retract to right
8) Place maleable retractor in RLQ and LLQ
9) small side wall retractor for abdominal wall to left
2) Midline incision from xiphi to pubis
3) Check placement of NG
4) Find and divide LT and mobilize 4th part of duodenum by dividing filmy attachment between duodenum and inferior mesenteric vein
5) Place bookwalter or omni with right sided bias as most contents will be retracted that way
6) Retract tranverse colon by placing splancnic retractors to also retract duodenum and IMV
7) Place large maleable retractor at base of small bowel mesentery and retract to right
8) Place maleable retractor in RLQ and LLQ
9) small side wall retractor for abdominal wall to left
Glasgow Coma Scale (GCS)
Adults: EVM (456):
Eyes:
1- none
2- open to pain
3- open to voice
4- spontaneously
Verbal:
1- none/intubated
2- incomprehensible
3- inappropriate
4- confused
5- oriented
Movement:
1- none
2- decorticate posturing
3- decrebrate posturing
4- withdraws from pain
5- localizes to pain
6- spontaneous
Eyes:
1- none
2- open to pain
3- open to voice
4- spontaneously
Verbal:
1- none/intubated
2- incomprehensible
3- inappropriate
4- confused
5- oriented
Movement:
1- none
2- decorticate posturing
3- decrebrate posturing
4- withdraws from pain
5- localizes to pain
6- spontaneous
Monday, January 4, 2010
Buerger's Disease
AKA: Thromboangitis obliterans
- non-atherosclerotic, segmental inflammatory disease that affects small and medium sized arteries and veins of the extremities.
- affected patients are almost uniformly smokers to the point where somking is more or less a pre-requisite for this diagnosis.
Presentation:
- ischemia of distal small arteries and veins
- claudication of distal extremities, two or more limbs always involved
- differentiate from claudicants who have calf cramping typically
- progression leads to ischemic rest pain and ulceration of fingers and toes
Diagnosis:
- rule out: scleroderma, CREST, mixed connective-tissue disease, SLE, hypercoaguability disorders with serum screens (CBCD, lytes, BUN, Cr, LFTs, BG, UA, sed rate, CRP, hypercoagubility screen incl APAb, ANA, RF, Complement, SCL-70, anticentromere Ab)
- angiography (MRA or CTA) may be needed
- echo to rule out proximal embolic source
Treatment:
- stop smoking!!
- limited options if arterial occlusion has developed +/- ulceration
- calcium channel blockers may be useful if pt has developed Raynaud's phenomenon
- Revascularization is not an option as distal targets and saphenous conduits are toast
- Although graft patency rates are low if targets are available, if it heals ulcer usually results in high rate of limb salvage.
- Amputations inevitable in pts with extensive gangrene or sepsis
- non-atherosclerotic, segmental inflammatory disease that affects small and medium sized arteries and veins of the extremities.
- affected patients are almost uniformly smokers to the point where somking is more or less a pre-requisite for this diagnosis.
Presentation:
- ischemia of distal small arteries and veins
- claudication of distal extremities, two or more limbs always involved
- differentiate from claudicants who have calf cramping typically
- progression leads to ischemic rest pain and ulceration of fingers and toes
Diagnosis:
- rule out: scleroderma, CREST, mixed connective-tissue disease, SLE, hypercoaguability disorders with serum screens (CBCD, lytes, BUN, Cr, LFTs, BG, UA, sed rate, CRP, hypercoagubility screen incl APAb, ANA, RF, Complement, SCL-70, anticentromere Ab)
- angiography (MRA or CTA) may be needed
- echo to rule out proximal embolic source
Treatment:
- stop smoking!!
- limited options if arterial occlusion has developed +/- ulceration
- calcium channel blockers may be useful if pt has developed Raynaud's phenomenon
- Revascularization is not an option as distal targets and saphenous conduits are toast
- Although graft patency rates are low if targets are available, if it heals ulcer usually results in high rate of limb salvage.
- Amputations inevitable in pts with extensive gangrene or sepsis
Lymphedema
Occurs when there is impaired uptake of lmphatics
- increases interstitial oncotic pressures and perpetuates egress of lymph fluid
- remaining lymphatics dilate and develop valvular incompetence over time
- fibrosis of lymphatic walls eventually obilterates lymphatic channels
Skin thickens over time if lymphedema is not treated
- epidermis develops thick scaly deposits
- cracks in thickened epidermis can lead to cellulitis/lymphangitis
- may progress to malignant degeneration to lymphoscarcoma (rare): Stewart-Treves syndrome
- Lymphoscarcoma presents with reddish-purple discoloration or nodule, tends to form satellite lesions
- treatment of lymphosarcoma involves radical amputation, poor prognosis
![[angiosarcoma+nodule+2.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEgKR4XpNv7qSQyFY6VwrGvRZ0Y5THHMiljKvYTxQogAeZpx5UHPku37xUK8H35uFp1i5Y-Cro_Y-Jko1JmLjw4ZJU60_9EHbHGFfGhbWpXcRgGYg1ph5CIaJn-D5vzyDx0JbsCniPibz5k/s200/angiosarcoma+nodule+2.jpg)
Stewart-Treves Syndrome
Etiology:
- primary vs. secondary
Primary:
- all types more common in females
- Lymphedema I (Millroy's disease): present at birth, affects dorsum of foot, not typically progressive
- Lymphedema II (Lymphadema Praecox/Meige's disease): onset at puberty, most common form of lymphedema (65-80%). Affects lower extremities, unilateral. Peripheral lymphatics are hypoplastic.
- Lymphedema III (lymphedema tarda): presents in midlife (>35yo). Lower extremities.
Secondary:
- infection, cancer, morbid obesity
- worldwide, most common cause is infection with parasite (Wuchereria bancrofti)
Diagnosis:
- basic history and physical
- rule out other causes of lymphedema (cardiac, venous, renal, hepatic, iliac compression)
- if imaging desired then lymphoscintigraphy can be used to demonstrate decrerased clearance of lymph
Treatment:
conservative management predominates
- stop the positive feedback cycle of inflammation, infection and fibrosis
- skin hygeine, treatment of infection
- massage protocols to decompress limb followed by compression stockings if arterial supply is sufficient
medical treatment is limited:
- Abx to treat infection
- use of diuretics and benzopyrene (increase proteolysis in edema) are of questionable benefit
surgical management is described but rarely of benefit:
- debulking procedures (reduce size and weight of limb) - however, will also disrupt what lymph channels remain
- physiologic procedures attempt to reestablish lymphatic flow - long-term outcomes not good overall.
- increases interstitial oncotic pressures and perpetuates egress of lymph fluid
- remaining lymphatics dilate and develop valvular incompetence over time
- fibrosis of lymphatic walls eventually obilterates lymphatic channels
Skin thickens over time if lymphedema is not treated
- epidermis develops thick scaly deposits
- cracks in thickened epidermis can lead to cellulitis/lymphangitis
- may progress to malignant degeneration to lymphoscarcoma (rare): Stewart-Treves syndrome
- Lymphoscarcoma presents with reddish-purple discoloration or nodule, tends to form satellite lesions
- treatment of lymphosarcoma involves radical amputation, poor prognosis
![[angiosarcoma+nodule+2.jpg]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEgKR4XpNv7qSQyFY6VwrGvRZ0Y5THHMiljKvYTxQogAeZpx5UHPku37xUK8H35uFp1i5Y-Cro_Y-Jko1JmLjw4ZJU60_9EHbHGFfGhbWpXcRgGYg1ph5CIaJn-D5vzyDx0JbsCniPibz5k/s200/angiosarcoma+nodule+2.jpg)
Stewart-Treves Syndrome
Etiology:
- primary vs. secondary
Primary:
- all types more common in females
- Lymphedema I (Millroy's disease): present at birth, affects dorsum of foot, not typically progressive
- Lymphedema II (Lymphadema Praecox/Meige's disease): onset at puberty, most common form of lymphedema (65-80%). Affects lower extremities, unilateral. Peripheral lymphatics are hypoplastic.
- Lymphedema III (lymphedema tarda): presents in midlife (>35yo). Lower extremities.
Secondary:
- infection, cancer, morbid obesity
- worldwide, most common cause is infection with parasite (Wuchereria bancrofti)
Diagnosis:
- basic history and physical
- rule out other causes of lymphedema (cardiac, venous, renal, hepatic, iliac compression)
- if imaging desired then lymphoscintigraphy can be used to demonstrate decrerased clearance of lymph
Treatment:
conservative management predominates
- stop the positive feedback cycle of inflammation, infection and fibrosis
- skin hygeine, treatment of infection
- massage protocols to decompress limb followed by compression stockings if arterial supply is sufficient
medical treatment is limited:
- Abx to treat infection
- use of diuretics and benzopyrene (increase proteolysis in edema) are of questionable benefit
surgical management is described but rarely of benefit:
- debulking procedures (reduce size and weight of limb) - however, will also disrupt what lymph channels remain
- physiologic procedures attempt to reestablish lymphatic flow - long-term outcomes not good overall.
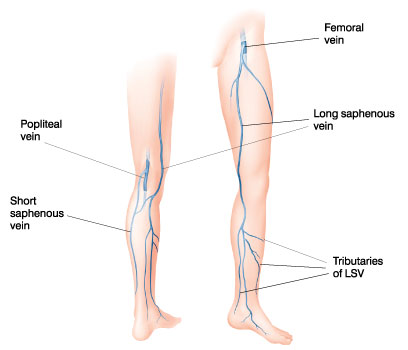
Short Saphenous Vein
- passes behind distal end of fibula (lateral malleolus) up the back of the leg to penetrate the deep fascia and join the popliteal vein
- medial sural cutaneous closely approximates the short saphenous and care must be taken to avoid it (Plate 468 Netter's)
- medial sural cutaneous nerve harvested as a cable graft for facial nerve when resected along with parotid.
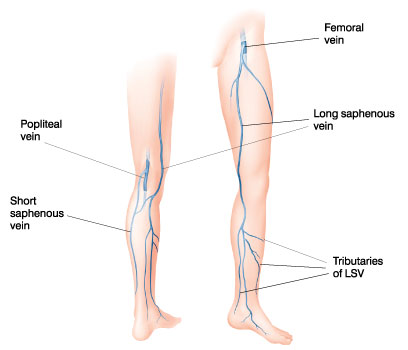
- medial sural cutaneous closely approximates the short saphenous and care must be taken to avoid it (Plate 468 Netter's)
- medial sural cutaneous nerve harvested as a cable graft for facial nerve when resected along with parotid.
Nutrition Academic Half-Day:
Dumping Syndrome:
- 4-6 small meals a day
- Avoid liquids with meals
- liquids 30 mins after a meal
- avoid high sugar foods
Bariatrics:
- full fluids for 2 weeks post-op
- avoid carbonated drinks, caffeine, EToH
- high protein choices
- 1/2 cup fluids while pt awake
- transition to solids 2 weeks post-op
- 3 meals with snacks in between
- drink milk between meals to incrase Ca and protein intake
- start 1/4 cup at a time, in crease to 1 cup (6-8 weeks)
- no drinking with meal/solids (so they don't fill up with low nutrient fluids)
- daily multivitamin
- calcium citrate with Vit D (Citrate is only form of calcium absorbed in the stomach)
- 1200-1500 IU Ca
- 800 U Vit D
Subscribe to:
Comments (Atom)