Definition: normal lining of the esophagus is replaced by a type of lining normally found in the intestines (this is called intestinal metaplasia) as evidenced by the prescence of goblet cells.
- Occurs in ~10% of pts with GERD
- important to differentiate between short (<3cm) vs long (>3cm) Barrett's
- there is debate whether short segment Barretts is actually associated with a risk of metaplasia
- annual risk of adenoca in Barrett's is 0.8%/yr
- risk of metaplasia in long segment is high - 90%
- if high grade dysplasia found - risk of invasive focus is 50%
Pts with Barrett's Surgical Rx to manage reflux may be more important.
- medical therapy does not result in regression of Barrett's while there is some evidence that surgical therapy does result in regression of Barrett's
- Surgery may prevent the progression of metaplasia to dysplasia and subsequently cancer
- Medical therapy does not prevent alkaline reflux - whereas surgical therapy does and this may be a contributing factor to the presence of Barrett's
Wednesday, November 25, 2009
Workup of GERD
Preoperative W/U in patients with classic symptoms of GERD:
- EGD
- Manometry
Pts with more complex symptoms consider:
- EGD
- Manometry
- 24 hr pH monitor
- Barium swallow
- impedence study
Demeester scoring:
...
- EGD
- Manometry
Pts with more complex symptoms consider:
- EGD
- Manometry
- 24 hr pH monitor
- Barium swallow
- impedence study
Demeester scoring:
...
Tuesday, November 24, 2009
Lower Limb Fasciotomy
4 compartment lower limb fasciotomy
Compartments of the lower limb:
1) Anterior Compartment:
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- peroneus tertius mm.
- deep peroneal nerve
- anterior tibilalis atery and venae communicantes
2) Lateral Compartment
- Peroneus longus m
- Peroneus brevis m.
- Superficial peroneal n.
3) Posterior Compartment:
- soleus m.
- gastrocnemius m.
- Palntatris tendon
4) Deep Posterior Compartment:
- Flexor hallicus longus
- Tibialis posterior
- Flexor digitorum longus mm.
- Tibial nerve
- Posterior tibial artery and venae communicantes
4 compartment fasciotomy involves 2 longitudinal incisions ~30 cm long. Anterior and Lateral compartments are decompressed with a lateral incision ~2cm anterior to fibula. 6-8 cm skin flaps are raised. Anterior compartment is decompressed with 25cm longitudinal incision lateral to the anterior edge of the tibia. Make a transverse incision in the fascia to find the intermuscular septum then the lateral compartment decompressed with a 25cm longitudinal incision in the fascia 1cm posterior to the intermuscular septum.
The Posterior and Deep Posterior compartments are then decompressed with a 30 cm longitudinal skin incision 2cm posterior to the tibia. 6-8 cm skin flaps are raised. The posterior compartment is decompressed with a 25 cm incision in the fascia 2 cm posterior to the posterior border of the tibia. The deep posterior compartment is accessed by dividing the soleus muscle off of the posterior border of the tibia and performing a 25 cm longitudinal incision posterior to the posterior border of the tibia. Watch out for the posterior tibial artery and venae communicantes lower in the leg in the deep posterior compartment
Compartments of the lower limb:
1) Anterior Compartment:
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- peroneus tertius mm.
- deep peroneal nerve
- anterior tibilalis atery and venae communicantes
2) Lateral Compartment
- Peroneus longus m
- Peroneus brevis m.
- Superficial peroneal n.
3) Posterior Compartment:
- soleus m.
- gastrocnemius m.
- Palntatris tendon
4) Deep Posterior Compartment:
- Flexor hallicus longus
- Tibialis posterior
- Flexor digitorum longus mm.
- Tibial nerve
- Posterior tibial artery and venae communicantes
4 compartment fasciotomy involves 2 longitudinal incisions ~30 cm long. Anterior and Lateral compartments are decompressed with a lateral incision ~2cm anterior to fibula. 6-8 cm skin flaps are raised. Anterior compartment is decompressed with 25cm longitudinal incision lateral to the anterior edge of the tibia. Make a transverse incision in the fascia to find the intermuscular septum then the lateral compartment decompressed with a 25cm longitudinal incision in the fascia 1cm posterior to the intermuscular septum.
The Posterior and Deep Posterior compartments are then decompressed with a 30 cm longitudinal skin incision 2cm posterior to the tibia. 6-8 cm skin flaps are raised. The posterior compartment is decompressed with a 25 cm incision in the fascia 2 cm posterior to the posterior border of the tibia. The deep posterior compartment is accessed by dividing the soleus muscle off of the posterior border of the tibia and performing a 25 cm longitudinal incision posterior to the posterior border of the tibia. Watch out for the posterior tibial artery and venae communicantes lower in the leg in the deep posterior compartment
Arterial Anatomy of the Extremities
Lower Extremity
1- aorta
2- common iliac
3- internal iliac
4- external iliac
5- femoral
6- profunda femoris
7- superficial femoral
8- popliteal
9- anterior tibial
10 -tibioperoneal trunk
11- peroneal
12- posterior tibial
13- dorsalis pedis arch
1- aorta
2- common iliac
3- internal iliac
4- external iliac
5- femoral
6- profunda femoris
7- superficial femoral
8- popliteal
9- anterior tibial
10 -tibioperoneal trunk
11- peroneal
12- posterior tibial
13- dorsalis pedis arch
Peripheral Vascular Disease
Claudication: cramping muscle pain or weakness produced by walking and relieved promptly by rest.
Rest pain: more sinister sign of CLI than night pain as gravity no longer improves symptoms of limb ischemia.
Night pain: pain in the toes at night while pt is supine.

Rest pain: more sinister sign of CLI than night pain as gravity no longer improves symptoms of limb ischemia.
Night pain: pain in the toes at night while pt is supine.
Thoracic outlet syndrome
Compression of the venous, arterial or nervous structures that pass out of the thoracic outlet can cause symptoms.
Diagnosis:
- there is no accepted set of diagnostic tests
Diagnosis:
- there is no accepted set of diagnostic tests
Saturday, November 21, 2009
Abdominal Aortic Aneurysm
- Expands at a rate of 0.4 cm/yr. This rate is dependent on a number of factors including aneurysm size, diastolic blood pressure, presence of COPD.
- Risk of rupture for a 5.0-5.5 cm aneurysm is 40% at 5 years
Indications for Operation:
- 5.0-5.5 cm in size
- rate of expansion > 0.5-1.0 cm/yr
- Risk of rupture for a 5.0-5.5 cm aneurysm is 40% at 5 years
Indications for Operation:
- 5.0-5.5 cm in size
- rate of expansion > 0.5-1.0 cm/yr
Friday, November 20, 2009
Surgical Management of GERD
Key Steps in Fundoplication:
1) Complete dissection of the esophageal hiatus and both crurae
2) Complete mobilization of the gastric fundus (+/- division of the short gastrics)
3) Closure of the hiatal defect
4) Creation of a tensionless wrap around a 50-60 Fr Bougie
5) Limiting the length of the wrap to 1.5-2.0 cm
6) Stabilizing the wrap to the esophagus with partial thickness bites of the esophagus while securing the wrap.
Complications of Fundo:
- 5-10% solid food dysphagia
- 2-3% have permenant dysphagia
- 7-10% have gas bloat, diarrhea, nausea, early satiety
- c/in 3-5 years some PTA are back on PPIs
Short Gastric Vessels:
- Study from Australia that demonstrates that there is no benefit to routinely taking the short gastrics
Variations to Fundoplication:
- Collis gastroplasty: used in setting of shortened esophagus. Rarely indicated. Be aware that 80% of pts are prone to esophagitis and pathologic esophageal acid exposure as a result.
- Toupet Fundoplication: 270-degree wrap where edges of fundus are secured to the lateral esophagus. Used in the setting of pts with abnormal esophageal motility to prevent dysphagia and bloating.
Post-operative retching:
- patients are treated aggressively with anti-nauseants to prevent post-op N&V. Should the pt have an espisode of N/V then a barium swallow should be performed to r/o wrap herniation or disruption. If this is caught within 24-48 hrs then re-operation can be performed. Otherwise 8-12 weeks should be allowed prior to any re-intervention.
Surgical Outcomes:
Spelcher, NEJM 1992: PPI vs open surgery (RCT, n~250)
- Open Nissen vs upto 4 meds for complicated GERD
- Both PPI and surgery effective in decreasing Sx and Esophagitis over 2 years - although surgery saw better improvements.
Spechler, JAMA 2001: Long-term results
- ~60% were back on PPI after 10yrs
- no difference was seen in rates of esophagitis in surgery and PPI groups.
- Pts should put this long term data into perspective when contemplating surgery.
Laparoscopic outcomes:
- >93% symptom free after 1 yr
- Transient dysphagia seen in 50% of pts - resolves within 3 weeks
- Long-term dysphagia seen ~10% of pts but well tolerated by most
- 3-4% require reoperation for unrelenting dysphagia or recurrent GERD
- Gas bloat avoided by floppy fundo
- Posted from iPhone
1) Complete dissection of the esophageal hiatus and both crurae
2) Complete mobilization of the gastric fundus (+/- division of the short gastrics)
3) Closure of the hiatal defect
4) Creation of a tensionless wrap around a 50-60 Fr Bougie
5) Limiting the length of the wrap to 1.5-2.0 cm
6) Stabilizing the wrap to the esophagus with partial thickness bites of the esophagus while securing the wrap.
Complications of Fundo:
- 5-10% solid food dysphagia
- 2-3% have permenant dysphagia
- 7-10% have gas bloat, diarrhea, nausea, early satiety
- c/in 3-5 years some PTA are back on PPIs
Short Gastric Vessels:
- Study from Australia that demonstrates that there is no benefit to routinely taking the short gastrics
Variations to Fundoplication:
- Collis gastroplasty: used in setting of shortened esophagus. Rarely indicated. Be aware that 80% of pts are prone to esophagitis and pathologic esophageal acid exposure as a result.
- Toupet Fundoplication: 270-degree wrap where edges of fundus are secured to the lateral esophagus. Used in the setting of pts with abnormal esophageal motility to prevent dysphagia and bloating.
Post-operative retching:
- patients are treated aggressively with anti-nauseants to prevent post-op N&V. Should the pt have an espisode of N/V then a barium swallow should be performed to r/o wrap herniation or disruption. If this is caught within 24-48 hrs then re-operation can be performed. Otherwise 8-12 weeks should be allowed prior to any re-intervention.
Surgical Outcomes:
Spelcher, NEJM 1992: PPI vs open surgery (RCT, n~250)
- Open Nissen vs upto 4 meds for complicated GERD
- Both PPI and surgery effective in decreasing Sx and Esophagitis over 2 years - although surgery saw better improvements.
Spechler, JAMA 2001: Long-term results
- ~60% were back on PPI after 10yrs
- no difference was seen in rates of esophagitis in surgery and PPI groups.
- Pts should put this long term data into perspective when contemplating surgery.
Laparoscopic outcomes:
- >93% symptom free after 1 yr
- Transient dysphagia seen in 50% of pts - resolves within 3 weeks
- Long-term dysphagia seen ~10% of pts but well tolerated by most
- 3-4% require reoperation for unrelenting dysphagia or recurrent GERD
- Gas bloat avoided by floppy fundo
- Posted from iPhone
Prosthetic repair ventral hernias
Dr. Bendavid - Montreal
Stoppa - preperitobeal mesh placement. Wjs 1989 13:545. Study performed by experts
- Posted from iPhone
Stoppa - preperitobeal mesh placement. Wjs 1989 13:545. Study performed by experts
- Posted from iPhone
Wednesday, November 18, 2009
Morton, NEJM 2006
Groups:
· wide excision with SLNB (biopsy)
· wide excision and observation of regional nodal basin (obs)
o underwent delayed lymphadenectomy if nodal recurrences became clinically detectable
· It’s an interim analysis of a multi-centre study comparing SLNB with clinical observation (q3 months) of the regional drainage basin.
· Basically, the point is, SLNB good, observation bad because once these patients develop clinically evident disease, therapeutic resection at that point carries a higher mortality.
Link:
Oral Exam Questions - Fall 2009
- Discuss neoadjuvant and surgical therapy for T3N0 rectal cancer patient
- Discuss surgical management for 1.8mm thick calf melanoma previously excised with positive margins
- Describe ER and operative management of unstable RUQ stabbing patient with liver laceration and anterolateral duodenal injury.
Groin Dissection for Melanoma
Describe groin dissection for melanoma ...
borders of femoral triangle
- inguinal ligament
- sartorius
- adductor longus muscle
borders of femoral triangle
- inguinal ligament
- sartorius
- adductor longus muscle
Indications for SLNB for Melanoma
- >1mm thickness
- <1mm thickness, BUT ulcerated
- <1mm thickness, BUT Clark's level 4-5
- lesions with unknown depth of invasion
- lesions with regression
- <1mm thickness, BUT ulcerated
- <1mm thickness, BUT Clark's level 4-5
- lesions with unknown depth of invasion
- lesions with regression
Classification of Melanoma Metastases
Satellite Metastases:
- metastatic disease within 2cm of primary lesion
In Transit Metastases:
- distant mets >2cm from primary disease
- metastatic disease within 2cm of primary lesion
In Transit Metastases:
- distant mets >2cm from primary disease
Melanoma Subtypes
If you are walking on the "LANDS" you'll get melanoma
Lentigo maligna
-less common 10%
- slow growing and large
Acral Lentiginous
- rare 1-5%
Nodular Sclerosing
- 2nd most common 15-30%
- aggressive and develop rapidly
Desmoplastic
- wider margins advocated
Superficial Spreading
- most common 70%
- not necessarily associated with sun exposed skin
Lentigo maligna
-less common 10%
- slow growing and large
Acral Lentiginous
- rare 1-5%
Nodular Sclerosing
- 2nd most common 15-30%
- aggressive and develop rapidly
Desmoplastic
- wider margins advocated
Superficial Spreading
- most common 70%
- not necessarily associated with sun exposed skin
Breast Cancer Staging
T1: <2cm
T2: 2-5 cm
T3: >5 cm
T4a: invades into pec major or chest wall
T4b: invades into skin
T4c: inflammatory breast cancer
N0: no nodes
N1: palpable mobile LN
N2: palpable fixed LN
N3: supraclavicular LN
T2: 2-5 cm
T3: >5 cm
T4a: invades into pec major or chest wall
T4b: invades into skin
T4c: inflammatory breast cancer
N0: no nodes
N1: palpable mobile LN
N2: palpable fixed LN
N3: supraclavicular LN
| Stage | T1 | T2 | T3 | T4 |
| N0 | 1 | 2a | 2b | 3b |
| N1 | 2a | 2b | 3a | |
| N2 | 3a | |||
| N3 | 3c | |||
Colon Cancer Staging
Stage 1: T1N0 or T2N0
Stage 2: T3N0 or T4N0
Stage 3: Any T, N1 or 2
Stage 4: Any T, Any N, M1
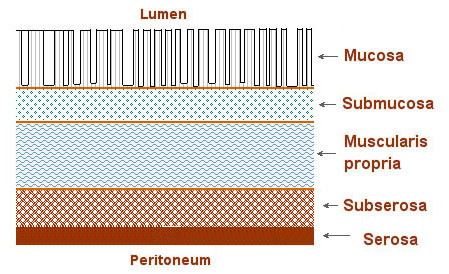
T1: invades into submucosa
T2: invades into muscularis propria
T3: invades through muscularis propria into subserosa or non-peritonealized pericolonic tissue
T4: invades through serosa into adjacent organs
N0: 0 LN mets (min 12 LN sampled)
N1: 1-3 LN
N2: >=4 LN
Stage 2: T3N0 or T4N0
Stage 3: Any T, N1 or 2
Stage 4: Any T, Any N, M1
T1: invades into submucosa
T2: invades into muscularis propria
T3: invades through muscularis propria into subserosa or non-peritonealized pericolonic tissue
T4: invades through serosa into adjacent organs
N0: 0 LN mets (min 12 LN sampled)
N1: 1-3 LN
N2: >=4 LN
Anastrazole
Aromatase inhibitor used in Breast ca patients who have progressed on tamoxifen.
- inhibits the production of estrogen
Well tolerated drug
- inhibits the production of estrogen
Well tolerated drug
Trastuzumab
Aka: Herceptin
Humanized mAb against her2/neu growth factor receptor expressed on many breast ca tumor cells.
- exact mechanism unknown.
Mild SE common:
- fever, chills, N&V, headache
- worsens leukopenia, anemia and diarrhea when given in combination with other chemotherapeutics
Humanized mAb against her2/neu growth factor receptor expressed on many breast ca tumor cells.
- exact mechanism unknown.
Mild SE common:
- fever, chills, N&V, headache
- worsens leukopenia, anemia and diarrhea when given in combination with other chemotherapeutics
Tamoxifen
Anti-estrogen used primarily for breast ca.
- inhibits estrogen stimulation of estrogen dependent tumors
Usually well tolerated. SE associated with estrogen inhibition (ie: hot flashes, weight gain, mood changes)
- inhibits estrogen stimulation of estrogen dependent tumors
Usually well tolerated. SE associated with estrogen inhibition (ie: hot flashes, weight gain, mood changes)
Imatinib
Aka: Gleevec
Tyrosine Kinase used for metastatic and recurrent GIST. Was developed for CML.
- inhibits tyr kinase receptors c-kit
No real dose-limiting toxicities:
- hepatotoxicity occurs but just need to follow LFTs
- mild SE like fluid retention, N&V, diarrhea
Tyrosine Kinase used for metastatic and recurrent GIST. Was developed for CML.
- inhibits tyr kinase receptors c-kit
No real dose-limiting toxicities:
- hepatotoxicity occurs but just need to follow LFTs
- mild SE like fluid retention, N&V, diarrhea
Paclitaxel
Aka: Taxol
Plant based taxane molecule used for breast cancer. Also used in lung, H&N ca.
- binds tubules of cells and prevents rapidly proliferating cells from replicating
Myelosuppression (neutropenia) predominates and is usually dose-limiting.
Other common less severe SE:
- mucositis, peripheral neuropathy, cardiac SE (HTN, hypotn, arrythmias), alopecia
Plant based taxane molecule used for breast cancer. Also used in lung, H&N ca.
- binds tubules of cells and prevents rapidly proliferating cells from replicating
Myelosuppression (neutropenia) predominates and is usually dose-limiting.
Other common less severe SE:
- mucositis, peripheral neuropathy, cardiac SE (HTN, hypotn, arrythmias), alopecia
Oxaliplatin
New generation platinum based chemotherapeutic used for metastatic colon ca.
- crosslinks and damages DNA
Like cisplatin, nephro and neurotoxicity are the most common dose-limiting side-effects.
Myelosuppression is expected but only sometimes dose limiting.
- crosslinks and damages DNA
Like cisplatin, nephro and neurotoxicity are the most common dose-limiting side-effects.
Myelosuppression is expected but only sometimes dose limiting.
Mitomycin C
Antitumor antibiotic used in gastric adenoca, pancreatic, breast and lung ca.
- inhibits DNA and RNA synthesis
Myelosuppression is common and dose-limiting.
- nadir seen at 4 weeks with recovery of WBC at 6-7 weeks
Other common SE include:
- N&V, anorexia and fatigue
- inhibits DNA and RNA synthesis
Myelosuppression is common and dose-limiting.
- nadir seen at 4 weeks with recovery of WBC at 6-7 weeks
Other common SE include:
- N&V, anorexia and fatigue
Methotrexate
Antifolate antimetabolite used in both benign and malignant diseases. Notably IBD, Breast ca, SCC and sarcomas.
- inhibits dihydrofolate reductase preventing nucleotide synthesis
Myelosuppression is the most common SE and is dose-limiting
- inhibits dihydrofolate reductase preventing nucleotide synthesis
Myelosuppression is the most common SE and is dose-limiting
Irinotecan
Topoisomerase I inhibitor used in recurrent and refractory colon ca in combination with 5-FU.
- Topoisomerases unwind DNA to allow is to be replicated.
Myelosuppression with neutropenia is common and dose limiting.
Diarrhea is also common and can be dose-limiting.
- Topoisomerases unwind DNA to allow is to be replicated.
Myelosuppression with neutropenia is common and dose limiting.
Diarrhea is also common and can be dose-limiting.
Gemcitibine
Nucleoside analogue used in advanced pancreatic and metastatic breast ca
- causes S-phase arrest as it prevents DNA synthesis
Myelosuppression and anemia are mild but dose limiting
- causes S-phase arrest as it prevents DNA synthesis
Myelosuppression and anemia are mild but dose limiting
5-Fluorouracil
Pyrimidine antimetabolite used for colon, rectum, gastric, pancreatic and breast cancer.
- Inhibits thymidylate synthase which prevents DNA and RNA synthesis. Enhanced by addition of leucovorin.
Side-effects:
- mucositis, diarrhea from epithelial cell turnover.
- hand-foot syndrome
- myelosuppression less with continuous infusions
- Inhibits thymidylate synthase which prevents DNA and RNA synthesis. Enhanced by addition of leucovorin.
Side-effects:
- mucositis, diarrhea from epithelial cell turnover.
- hand-foot syndrome
- myelosuppression less with continuous infusions
Doxorubicin
Aka: Adriamycin
Anthracycline based chemotherapeutic used for variety of cancers including breast cancer and sarcomas.
- Intercalates with DNA and is non-cell cycle specific.
Rate limiting toxicity is myelosuppression and cardiotoxicity.
- Cardiotoxicity usually presents as chronic cardiomyopathy after prolonged use. Acute cardiac arrythmias are rare
Anthracycline based chemotherapeutic used for variety of cancers including breast cancer and sarcomas.
- Intercalates with DNA and is non-cell cycle specific.
Rate limiting toxicity is myelosuppression and cardiotoxicity.
- Cardiotoxicity usually presents as chronic cardiomyopathy after prolonged use. Acute cardiac arrythmias are rare
Cisplatin
Platinum based compound used in almost every class of solid tumor.
- Thought to intercalate with DNA and disrupt replication
- Dose limiting toxicity is Nephrotoxicity
- After cumulative doses painful Neuropathy may also be dose limiting
- Chronic use can result in ototoxicity
- Thought to intercalate with DNA and disrupt replication
- Dose limiting toxicity is Nephrotoxicity
- After cumulative doses painful Neuropathy may also be dose limiting
- Chronic use can result in ototoxicity
Hand-Foot Syndrome
Common side-effect associated with 5-FU, although all anthracycline chemotherapeutics are metabolized to 5-FU and can cause this side-effect.
Characterized by tingling and pain in the palms and soles of feet. Swelling and erythema is usually associated.
Management is to lower or stop chemotherapeutic agent. Steroid creams may help to aleviate symptoms
Characterized by tingling and pain in the palms and soles of feet. Swelling and erythema is usually associated.
Management is to lower or stop chemotherapeutic agent. Steroid creams may help to aleviate symptoms
Desmoid Tumors
Difficult to treat desmoplastic reaction usually in mesentery.
- Associated with FAP
- Severity of desmoid reaction is inversely proportional to the number of polyps.
- therefore, some argue that pts with attenuated FAP with fewer polyps should have surgery delayed as long as possible to prolong the risk of developing post-op desmoid tumors
Treatment:
- treatment of desmoid tumors is limited.
- NO Surgery! Desmoplastic reaction only gets worse with each surgery
- only effective therapy is adriamycin based chemotherapy
- Associated with FAP
- Severity of desmoid reaction is inversely proportional to the number of polyps.
- therefore, some argue that pts with attenuated FAP with fewer polyps should have surgery delayed as long as possible to prolong the risk of developing post-op desmoid tumors
Treatment:
- treatment of desmoid tumors is limited.
- NO Surgery! Desmoplastic reaction only gets worse with each surgery
- only effective therapy is adriamycin based chemotherapy
Tuesday, November 17, 2009
Diagnostic Criteria for Lynch Syndrome
Amsterdam Criteria (3-2-1):
Amsterdam criteria was developed for research and therefore very specific criteria.
- 3 relatives with colon ca
- 2 generations
- 1 family member <50 yo
Modified Amsterdam and Bethesda criteria were subsequently developed to be further encompassing.
Modified Amsterdam Criteria:
- same as Amsterdam criteria but cancers can also include: colon, small bowel, ureter, renal pelvis and endometrial ca.
Bethesda Criteria:
- Amsterdam criteria or
- 2 cases of HNPCC cancers in 1 pt, including synch or metach CRC
- Colon CA and 1st deg relative with CA/adenoma (CA <45, adenoma <40)
- Colon or endometrial CA <45
- R sided colon CA with histo undiff, solid, cribiform, signet-cell <45
- Adenoma <40
Amsterdam criteria was developed for research and therefore very specific criteria.
- 3 relatives with colon ca
- 2 generations
- 1 family member <50 yo
Modified Amsterdam and Bethesda criteria were subsequently developed to be further encompassing.
Modified Amsterdam Criteria:
- same as Amsterdam criteria but cancers can also include: colon, small bowel, ureter, renal pelvis and endometrial ca.
Bethesda Criteria:
- Amsterdam criteria or
- 2 cases of HNPCC cancers in 1 pt, including synch or metach CRC
- Colon CA and 1st deg relative with CA/adenoma (CA <45, adenoma <40)
- Colon or endometrial CA <45
- R sided colon CA with histo undiff, solid, cribiform, signet-cell <45
- Adenoma <40
Lower GI Bleeding
Investigations:
- Success of imaging directed at identifying the source of bleeding will largely depend on the ongoing rate of bleeding.
- Angiogram: 0.5 cc/min
- RBC scan: 0.1 cc/min
- Success of imaging directed at identifying the source of bleeding will largely depend on the ongoing rate of bleeding.
- Angiogram: 0.5 cc/min
- RBC scan: 0.1 cc/min
Risk of Cancer in IBD
Risk increases significatntly 8 years after pancolitis:
Therefore, recommendation is to begin colonscopic screening 8 years after the onset of pancolitis.
- In patients with left-sided colitis only, screening can begin 12-15 years after the onset of disease.
Therefore, recommendation is to begin colonscopic screening 8 years after the onset of pancolitis.
- In patients with left-sided colitis only, screening can begin 12-15 years after the onset of disease.
Layers of Bowel Wall
- Lumen (interior surface of colon "tube")
- Mucosa
- Lamina propria or basement membrane—dividing line between in situ and invasive lesions
- Muscularis mucosae
- Submucosa—lymphatics; potential for metastases increases
- Muscularis propria
- Circular layer
- Longitudinal layer—in three bands called taenia coli
- Subserosa—sometimes called pericolic fat or subserosal fat
- Serosa—present on ascending, transverse, sigmoid only (also called the visceral peritoneum)
- Retroperitoneal fat (also called pericolic fat)
- Mesenteric fat (also called pericolic fat)
http://training.seer.cancer.gov/images/colorectal/layers.jpg
Haggitt Levels - Colonic Polyps
Describe invasion of invasive carcinoma in pedunculated colonic polyps. The Kudo classification is used to describe invasion in sessile polyps.
Level 0 - CIS (carcinoma confined to mucosal layer)
Invasion through Lamina propria:
Level 1 - invasion into submucosa limited to head of polyp
Level 2 - invasion into submucosa extending to neck of polyp
Level 3 - invasion into submucosa extending to stalk of polyp
Level 4 - invasion beyond the stalk but above the muscularis propria
Indications for Surgical Management of Polyps after Polypectomy:
- Positive margins
- Piecemeal resection
- Lymphovascular invasion
- Poorly differentiated
- Haggit level 4
- Unable to resect endoscopically
Level 0 - CIS (carcinoma confined to mucosal layer)
Invasion through Lamina propria:
Level 1 - invasion into submucosa limited to head of polyp
Level 2 - invasion into submucosa extending to neck of polyp
Level 3 - invasion into submucosa extending to stalk of polyp
Level 4 - invasion beyond the stalk but above the muscularis propria
Indications for Surgical Management of Polyps after Polypectomy:
- Positive margins
- Piecemeal resection
- Lymphovascular invasion
- Poorly differentiated
- Haggit level 4
- Unable to resect endoscopically
Monday, November 16, 2009
Diverticulitis
Diagnosis:
- CT is the primary modality by which diverticulitis is diagnosed. Resoltion of LLQ pain after a course of abx does not constitute evidence for an episode of diverticulitis.
- Pts should eventually undergo colonoscopy to rule out malignant processes, most wait 6-8 weeks to prevent blowing out a microperforation.
- 70% of cases of uncomplicated diverticulitis will resolve with medical therapy alone.
- CT is the primary modality by which diverticulitis is diagnosed. Resoltion of LLQ pain after a course of abx does not constitute evidence for an episode of diverticulitis.
- Pts should eventually undergo colonoscopy to rule out malignant processes, most wait 6-8 weeks to prevent blowing out a microperforation.
- 70% of cases of uncomplicated diverticulitis will resolve with medical therapy alone.
Hinchey Classification - Diverticulitis
When originally described based on laparotomy findings. Now it is applied to CT findings.
0: Diverticulosis, no evidence of inflammation
1: Pericolonic or mesenteric abscess
2: Contained pelvic abscess
3: Free purulent perforation
4: Free feculent perforation
Sunday, November 15, 2009
Diverticulitis - Indications for Surgery
Strong Evidence for Surgery:
- Diffuse peritonitis
- Free perforation
- Fistula
- Stricture
- Obstruction
- Immunocompromised patient
- >= 4 uncomplicated episodes
Conflicting Evidence for Surgery:
- After abscess drainage
- Uncomplicated, 2 or 3 episodes
Surgery No Longer Supports Surgery:
- Uncomplicated 1st episode
- Age <50
Broderick-Villa G, 2005: Large retrospective review examining pts with recurrent diverticulitis. After conservative treatment, few (13%) recurred and most of these recurrences were managed conservatively again.
- Diffuse peritonitis
- Free perforation
- Fistula
- Stricture
- Obstruction
- Immunocompromised patient
- >= 4 uncomplicated episodes
Conflicting Evidence for Surgery:
- After abscess drainage
- Uncomplicated, 2 or 3 episodes
Surgery No Longer Supports Surgery:
- Uncomplicated 1st episode
- Age <50
Broderick-Villa G, 2005: Large retrospective review examining pts with recurrent diverticulitis. After conservative treatment, few (13%) recurred and most of these recurrences were managed conservatively again.
Primary Hyperparathyroidism
Presentation:
- most present asymptomatically and come to attention after screening bloodwork reveals hypercalcemia.
- otherwise look for signs of hypercalcemia - stones, bones, psychiatric overtones, abdominal moans
Investigations:
- PTH, calcium, phosphate
- 24h urine calcium to differentiate for FHH
- 99Tc sestamibi and high resolution ultrasound.
- together these imaging tests will usually localize the lesion and allow for unilateral neck exploration.
- if not localized by above studies consider CT, MRI or PET scan
Indications to operate hyperpara:
- symptomatic - some would argue this includes vague symtpoms such as dysphoria and failure to thrive in the elderly
- serum calcium > 3 mmol/l
- 24h urine calcium > 400 mg/l
- age <50
- bone density < 2 sd
- unable yo follow up with medical observation
Unilateral exploration:
- should be accompanied ideally with intraop PTH assay.
- if not available then ?frozen section
- if PTH assay not available ?warn pt about possible need to return to explore other side
Perioperative Complications:
- hungry bone syndrome: if preop calcium was very high > 3, then there may be rapid bone reabsorption of calcium postoperative. May need yo give patient supplemental calcium postoperatively.
- severe hypercalcemia: may need to give IV palmidrobate infusion over 4 hours to decrease calcium. Effects can last days to weeks. If not sufficient the give IV bisphosphonates (inhibits osteoclastic bone reabsorption)
- most present asymptomatically and come to attention after screening bloodwork reveals hypercalcemia.
- otherwise look for signs of hypercalcemia - stones, bones, psychiatric overtones, abdominal moans
Investigations:
- PTH, calcium, phosphate
- 24h urine calcium to differentiate for FHH
- 99Tc sestamibi and high resolution ultrasound.
- together these imaging tests will usually localize the lesion and allow for unilateral neck exploration.
- if not localized by above studies consider CT, MRI or PET scan
Indications to operate hyperpara:
- symptomatic - some would argue this includes vague symtpoms such as dysphoria and failure to thrive in the elderly
- serum calcium > 3 mmol/l
- 24h urine calcium > 400 mg/l
- age <50
- bone density < 2 sd
- unable yo follow up with medical observation
Unilateral exploration:
- should be accompanied ideally with intraop PTH assay.
- if not available then ?frozen section
- if PTH assay not available ?warn pt about possible need to return to explore other side
Perioperative Complications:
- hungry bone syndrome: if preop calcium was very high > 3, then there may be rapid bone reabsorption of calcium postoperative. May need yo give patient supplemental calcium postoperatively.
- severe hypercalcemia: may need to give IV palmidrobate infusion over 4 hours to decrease calcium. Effects can last days to weeks. If not sufficient the give IV bisphosphonates (inhibits osteoclastic bone reabsorption)
Operative Repair of Hiatal Hernias
 Port placement:
Port placement: - 10mm umbo camera port
- 10 mm epigastric liver retraction port
- 5mm para-rectus operating ports
- 5mm R ant axill line fundal retraction port
- Description of procedure ...
Controversies:
- Fundoplication? Accepted for type 1 and 3 as they usually have significant reflux symptoms. Less clear for type 2 . Technically GE jxn is in abdomen - however, these patients may have subclinical symptoms of reflux. In general, addition of reflux procedure well accepted because it helps anchor the stomach in the abdomen to prevent hernia recurrence and type 2 pts may have subclinical sx that are unmasked by repair of hernia.
- Use of mesh: not of proven benefit, however with advent of surgisis mesh, risks associated with non-absorbable mesh averted and generally used now.
Long course neoadjuvant chemoRT for rectal cancer
Sauer et. al., NEJM 2004 - Pre-op vs Post-op ChemoRT for Rectal ca
- no difference in overall survival but improved local recurrence rate
in pts with long course therapy.
Protocol:
- Radiation 5d per week for five weeks
- continuous 5-FU infusion during weeks 1 and 5.
- surgery performed within 6 weeks of completion of therapy
- decreases local recurrence from 13% to 6% in T3, T4 or N1 disease compared to postoperative adjuvant therapy.
- there was also a decrease in treatment toxicity (40% vs 27%) compared to postoperative adjuvant therapy.
- But no difference in overall survival.
- no difference in overall survival but improved local recurrence rate
in pts with long course therapy.
Protocol:
- Radiation 5d per week for five weeks
- continuous 5-FU infusion during weeks 1 and 5.
- surgery performed within 6 weeks of completion of therapy
- decreases local recurrence from 13% to 6% in T3, T4 or N1 disease compared to postoperative adjuvant therapy.
- there was also a decrease in treatment toxicity (40% vs 27%) compared to postoperative adjuvant therapy.
- But no difference in overall survival.
Saturday, November 14, 2009
Hiatal Hernia
Classification:
- Type 1: Sliding hernia - Laxity of phrenoesophageal ligament allows GE jxn to slide into chest
- Type 2: paraesophageal hernia - fundus of the stomach slides above hiatus, but GE jxn remains in the abdomen
- Type 3: Combination - GE junction above the hiatus AND fundus/body herniated into the thorax
Type 4: advanced type 3 - same but with entire stomach or other organs herniated through hiatus
There is a distinction between the terms hiatal hernia and paraesophageal hernias - all of above are hiatal hernias, however, only type 2 and 3 hernias are truly para's
Presentation:
- true incidence of type 1 hernias unknown because many asymptomatic, type 2 and 3 are very rare (<1% of hiatal hernias are type 2/3)
- often times diagnosed incidentally during investigations for other reasons
- If symptoms are present, may include reflux or mechanical symptoms of esophageal obstruction - pain, fullness, dysphagia, bloating, respiratory sx)
- Anemia: results from chronic GI blood loss in 1/3 of pts. Caused by linear ulcerations of the gastric cardia and resolves after repair.
- Borchardt's triad: chest pain, retching with inability to vomit and inability to pass NG. Indicative of an incarcerated hiatal hernia.
Diagnosis:
- barium swallow
- pH, manometry: may be difficult to acquire and interpret due to changes in anatomy. May not be very useful in type 2 and 3 hernias.
- EGD
Indications for OR:
- Type 1 hernias: leave asymptomatic pts alone. Symptomatic patients should first have symptom-specific work-up and subsequently be considered for repair.
- Asymptomatic patients: asymptomatic para's historically thought to have 30% mortality rate. However, more recent series suggest that ~80% of pts will remain asymptomatic.
- Symptomatic patients: all symptomatic patients should be reapired. This includes patients with esophageal mucosal changes (esophagitis, Barrett's) or anemia.
- Type 1: Sliding hernia - Laxity of phrenoesophageal ligament allows GE jxn to slide into chest
- Type 2: paraesophageal hernia - fundus of the stomach slides above hiatus, but GE jxn remains in the abdomen
- Type 3: Combination - GE junction above the hiatus AND fundus/body herniated into the thorax
Type 4: advanced type 3 - same but with entire stomach or other organs herniated through hiatus
There is a distinction between the terms hiatal hernia and paraesophageal hernias - all of above are hiatal hernias, however, only type 2 and 3 hernias are truly para's
- true incidence of type 1 hernias unknown because many asymptomatic, type 2 and 3 are very rare (<1% of hiatal hernias are type 2/3)
- often times diagnosed incidentally during investigations for other reasons
- If symptoms are present, may include reflux or mechanical symptoms of esophageal obstruction - pain, fullness, dysphagia, bloating, respiratory sx)
- Anemia: results from chronic GI blood loss in 1/3 of pts. Caused by linear ulcerations of the gastric cardia and resolves after repair.
- Borchardt's triad: chest pain, retching with inability to vomit and inability to pass NG. Indicative of an incarcerated hiatal hernia.
Diagnosis:
- barium swallow
- pH, manometry: may be difficult to acquire and interpret due to changes in anatomy. May not be very useful in type 2 and 3 hernias.
- EGD
Indications for OR:
- Type 1 hernias: leave asymptomatic pts alone. Symptomatic patients should first have symptom-specific work-up and subsequently be considered for repair.
- Asymptomatic patients: asymptomatic para's historically thought to have 30% mortality rate. However, more recent series suggest that ~80% of pts will remain asymptomatic.
- Symptomatic patients: all symptomatic patients should be reapired. This includes patients with esophageal mucosal changes (esophagitis, Barrett's) or anemia.
Operative Management of Pheochromocytoma
"No-Touch" technique:
- ligate the central draining vein first to prevent secretion of catacholamines into the systemic circulation.
- "no-touch" also thought to prevent wide blood pressure swings.
Open technique:
- Advantages were to facilitate "no-touch" technique, permit bilateral and central exploration.
- however, with improvements in laparoscopic technique and pre-operative imaging, currently open technique reserved for large pheos and obviously malignant lesions.
Laparoscopic technique:
- Lateral Transperitoneal Lap Adrenalectomy is now the gold standard for most-benign appearing pheos <8cm in size.
- Right adrenal is easier to excise whereas left side requires more extensive visceral medialization or access to the lesser sac.
- describe laparoscopic right and left adrenalectomy...
Management of intraoperative complications:
- hypotension: phenylephrine or ephedrine and volume expansion
- hypertension: nitroprusside
- ventricular arrhythmia: lidocaine
Post-operative care:
- blood pressure will commonly be low (SBP<100) in 1st 12hrs post-op until the pre-op doses of alpha-blocker absorbed
- hold all anti-hypertensive medications post-op unless the pt was taking chronic B-blocker
- Specimen examined pathologically for DNA ploidy. Diploid tumors behave in malignant fashion, however, even 30% of nondiploid tumors will also recur.
- ligate the central draining vein first to prevent secretion of catacholamines into the systemic circulation.
- "no-touch" also thought to prevent wide blood pressure swings.
Open technique:
- Advantages were to facilitate "no-touch" technique, permit bilateral and central exploration.
- however, with improvements in laparoscopic technique and pre-operative imaging, currently open technique reserved for large pheos and obviously malignant lesions.
Laparoscopic technique:
- Lateral Transperitoneal Lap Adrenalectomy is now the gold standard for most-benign appearing pheos <8cm in size.
- Right adrenal is easier to excise whereas left side requires more extensive visceral medialization or access to the lesser sac.
- describe laparoscopic right and left adrenalectomy...
Management of intraoperative complications:
- hypotension: phenylephrine or ephedrine and volume expansion
- hypertension: nitroprusside
- ventricular arrhythmia: lidocaine
Post-operative care:
- blood pressure will commonly be low (SBP<100) in 1st 12hrs post-op until the pre-op doses of alpha-blocker absorbed
- hold all anti-hypertensive medications post-op unless the pt was taking chronic B-blocker
- Specimen examined pathologically for DNA ploidy. Diploid tumors behave in malignant fashion, however, even 30% of nondiploid tumors will also recur.
Pheochromocytoma
-Tumor arising from chromaffin cells and sustentacular cells of the adrenal medulla or extraadrenal paraganglia.
- Classically secrete epinephrine, norepinephrine or dopamine. However, can also secrete a host of other hormones.
- Distinction between benign and malignant is the presence of local invasion or presence of distant mets.
Presentation:
- Classic triad: (PHEo) Paroxysmal HTN, Palpatations, Headache, Excess sweating
- Most (90%) will present with some clinical manifestation, whereas 10% will present initially as an adrenal incidentaloma.
- Number of familial conditions associated with pheo - notably MEN2a and 2b.
Diagnosis:
- Most specific test is combination of 24 hr urine metanephrines and catacholamines.
- Plasma testing, while very sensitive, is very expensive and not as specific.
- Any elevated 24hr urine metanephrine or 2x normal 24 hr urine catacholamine result is considered positive.
- Many drugs (notably, TCAs) can falsely elevate urine catacholamines.
- CT abdo/pelvis most cost-effective method to localize pheo once diagnosed. However, other modlities such as MRI, MIBG scan, and PET scan may be used as adjunctive imaging tests.
- With newer contrast agents - precipitation of hypertensive crisis is not as much of a concern and non-contrast CT not necessary
Perioperative Management:
- Important step in operative management in order to prevent hypertensive crisis intra-op.
- Unopposed alpha-stimulation once pheo removed will cause vasoconstriction and decreased intravascular volume
- alpha-blockade should begin immediately once diagnosis is made
- Phenoxybenzamine started at 20-30 mg qD in divided doses. Increase dose until the pt is symptomatic with orthostatic hypotension and/or nasal stuffiness.
- in order to combat side-effects instruct pt to increase salt and fluid intake.
- Beta-blockade with propranolol can be added to manage tachycardia, arrythmias or ischemia
- Classically secrete epinephrine, norepinephrine or dopamine. However, can also secrete a host of other hormones.
- Distinction between benign and malignant is the presence of local invasion or presence of distant mets.
Presentation:
- Classic triad: (PHEo) Paroxysmal HTN, Palpatations, Headache, Excess sweating
- Most (90%) will present with some clinical manifestation, whereas 10% will present initially as an adrenal incidentaloma.
- Number of familial conditions associated with pheo - notably MEN2a and 2b.
Diagnosis:
- Most specific test is combination of 24 hr urine metanephrines and catacholamines.
- Plasma testing, while very sensitive, is very expensive and not as specific.
- Any elevated 24hr urine metanephrine or 2x normal 24 hr urine catacholamine result is considered positive.
- Many drugs (notably, TCAs) can falsely elevate urine catacholamines.
- CT abdo/pelvis most cost-effective method to localize pheo once diagnosed. However, other modlities such as MRI, MIBG scan, and PET scan may be used as adjunctive imaging tests.
- With newer contrast agents - precipitation of hypertensive crisis is not as much of a concern and non-contrast CT not necessary
Perioperative Management:
- Important step in operative management in order to prevent hypertensive crisis intra-op.
- Unopposed alpha-stimulation once pheo removed will cause vasoconstriction and decreased intravascular volume
- alpha-blockade should begin immediately once diagnosis is made
- Phenoxybenzamine started at 20-30 mg qD in divided doses. Increase dose until the pt is symptomatic with orthostatic hypotension and/or nasal stuffiness.
- in order to combat side-effects instruct pt to increase salt and fluid intake.
- Beta-blockade with propranolol can be added to manage tachycardia, arrythmias or ischemia
Ankle Brachial Index (ABI):
SBP Ankle (dorsalis pedis and post-tibial a) / SBP brachial pulse
(higher of two arms)
Normal - 1
Claudication - 0.5-1
Rest pain, tissue loss - <0.5
Non-healing ulcer <0.3
(higher of two arms)
Normal - 1
Claudication - 0.5-1
Rest pain, tissue loss - <0.5
Non-healing ulcer <0.3
Labels:
Vascular
Subscribe to:
Comments (Atom)